There was nothing there on the ultrasound screen, just my beautiful uterus – empty. There was the teeniest tiniest black spot that may have been the beginning of a sac, but it was so small my Doctor was not certain. She didn’t need to say anything for me to quickly realise that I was not one of the lucky 1%. My doctor checked my ovaries: my right one is still hyperstimulated from the IVF and I had some VERY big follicles/cysts (but this is normal for after IVF and of no concern, but may explain any pain I may have here), my left ovary too was swollen, but not as bad as my right one.
What does this mean? It was difficult for my doctor to say without knowing what my beta test results are. If my hCG levels are continuing to rise, it is likely that I have a tubal pregnancy (ectopic pregnancy – a pregnancy that grows outside of the uterus). If my hCG levels are falling, then it will be safe to assume that I have a chemical pregnancy* and the little black spot on the screen was indeed huckleberry.
My symptoms have been spotting dark brown blood since Friday, general abdominal pains all day Monday, my spotting surprisingly stopped today (Tuesday). I have had some pains specifically on my left side, although not overly sharp pains, and I pointed out to the doctor (doctors – there were 2 others in the room with her) where this was….yeh, about where my ovary/fallopian tubes are.
If this is a chemical pregnancy then the doctor will prescribe me some medication (a vaginal pessary, I cannot remember the name of it) to help my body along with expelling the uterine pregnancy. If this medication doesn’t work, or my hCG levels come back higher with a likelihood of a tubal pregnancy, then I will be prescribed Methotrexate (an intramuscular injection – YEY another injection, of course!!!). I want to avoid taking this drug because it will mean we are not allowed to conceive for at least another 3 months because the chemical can stay in the body and harm a developing embryo. But at the same time, we don’t want to wait and see for too long because there is a chance my tube could rupture and I would lose a fallopian tube. I have read that even after being given the shot their tube still ruptured because it was left too late.
So I was asking you to hope with me that I didn’t bleed, but now I want to bleed….please, please body, just bleed!!! I think this will be one of those times when I cry tears of happiness when I start to bleed full flow! I know it will also be sad at the same time….choo choo, all aboard the emotional train wreck!!!
I mentioned that there were two other doctors in the room, one was ‘shadowing’, the other was a fellow (no not a chappie you silly Brits!!!). The fellow interjected and answered some of our questions, he was clearly very knowledgeable, but there was a lot of bouncing around between them. Chris was getting frustrated with the information we were receiving, they were talking to us as if we were medical professionals. It took 5 minutes of Chris’s continued questioning to get the doctors to say that despite the miscarriage being bad (and sad), what we were seeing was ‘normal’ or ‘common’. What they really needed to start out with was – don’t worry, there is nothing seriously wrong with you, chemical pregnancies happen frequently with IVF (because they are transferring 2 embryos). I think I had a bit more knowledge than Chris and didn’t feel quite as frustrated because I had googled a lot on miscarriage, chemical pregnancy, blighted ovum and have read forums/blogs etc. So my lesson here is to share more of my ‘google expert medical opinion’ knowledge with Chris before these types of appointments.
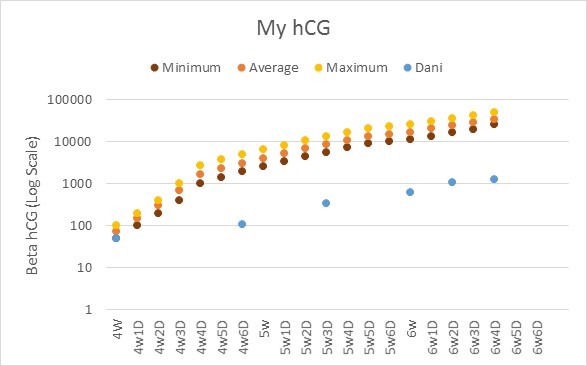
We also discussed my hCG levels (49, 110 and 345) and my doctor did admit that my first hCG result of 49 was borderline low- to non viable. So why, oh why, did the other doctor (who did my IUIs) seem so happy and chirpy on the phone, proceed to tell me my progesterone and estrogen levels were excellent but fail to tell me my hCG level. All it required was this: “Congratulations Ms Dani, you are pregnant, but your levels were a little lower than average, we would like to see you again in 5 days just to make sure you levels are doubling nicely. Your estrogen & progesterone levels are excellent, so this is a good thing.” Expectation management is not a bad thing.
So – we have one big question answered, I feel a relief, albeit a sad relief – there is no viable pregnancy. The next big question we wait for an answer is – is this a chemical pregnancy or a tubal pregnancy?
*A chemical pregnancy is a clinical term for a very early miscarriage. It happens before an ultrasound could even detect a heartbeat (before the 5th week of gestation). This occurs when an egg is fertilized but it does not implant on the uterine wall. Chemical pregnancies are actually quite common, occurring in 50 – 60% of first pregnancies. There are many possible causes of chemical pregnancy – inadequate uterine lining, low hormone levels, luteal phase defect, infection, or other unknown reasons. The most common assumption is that they are due to chromosomal problems in the developing foetus. This can result from poor sperm or egg quality, genetic abnormalities from either mother or father, or abnormal cell division of the foetus.